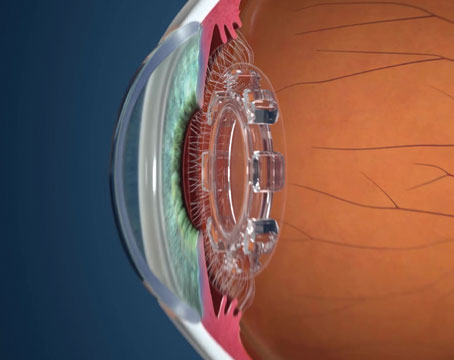
Dr. Michelson uses a familiar, relatively inexpensive instrument—the Maloney Astigmatism Keratometer (available from Storz and Katena)—to determine the astigmatic axis intraoperatively when he’s implanting toric lenses such as those from Alcon. “The Maloney keratometer is a qualitative instrument, designed by William Maloney, MD, to analyze astigmatism during basic phacoemulsification,” Dr. Michelson explains. “I’ve used it for about 20 years, especially when performing corneal transplants. In that situation, it allows me to look at suture-induced astigmatism intraoperatively and adjust the tension on the sutures to compensate. Now, I’m also using it when I implant toric lenses.”
 Determining the Axis
Determining the Axis
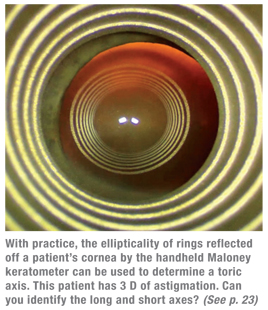
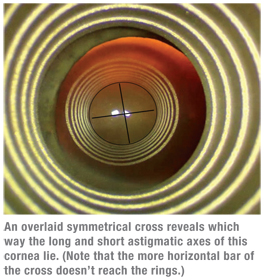
“The Maloney Keratometer is handheld,” explains Dr. Michelson. “You place it between the eye and the microscope. It projects a series of rings onto the cornea, much like a video keratoscope or placido disc during topography. The ellipticality of the reflection indicates the toricity of the cornea.
“When I know that a patient is a good candidate for a toric IOL, I import the videokeratoscope image from the Humphrey topographer into a PowerPoint presentation and print it out,” he says. “That lets me see how the astigmatism affects the shape of the central two to four rings where the line of vision lies. With a trained eye you can detect 1 D or more of astigmatism by noting the ellipticality of those rings. If I can see the ellipticality of the rings in the printout, I know I’ll be able to visualize the toricity intraoperatively with the keratometer and align the toric lens accurately.
“When we start surgery, the first thing I do is use the Maloney keratometer,” he continues. “I find the short axis of the ellipse, which marks the steep meridian, and the long axis. Then I find a corresponding landmark on the iris or limbus and use the marking pen there. The process is entirely visual and qualitative. The quantification of the astigmatism—how much needs to be corrected—occurs preoperatively during the refraction.”
Dr. Michelson says this approach has worked extremely well. “Of the hundreds of toric lenses I’ve put in, I’ve only had to readjust two or three that were about 10 degrees off,” he says. “We usually hit it right on the mark. In addition, I never have to mark a patient preop for a toric lens, and when using this approach it doesn’t matter whether the patient’s eye cyclotorts.” Dr. Michelson notes one caveat: “You need to avoid overflooding the cornea, which can produce a distorted mire,” he says. “You want to do this with just a thin meniscus of fluid on the cornea, and with the cul-de-sacs free of pooled fluid.”
Dr. Michelson didn’t always use this approach. “When toric lenses first became available, we marked patients’ eyes according to standard protocol,” he says. “But once I started using the Maloney keratometer, I didn’t see any reason to premark any more. It became unnecessary, and it was time-consuming to do it. Now my patients are brought into the operating room, anesthesia deals with them and then I’m ready to operate. I determine the astigmatic axis after we get the speculum in the eye.”
For the Average Surgeon?
Asim Piracha, MD, associate clinical professor in the University of Louisville Department of Ophthalmology and Visual Sciences and medical director of the John-Kenyon American Eye Institute in Louisville, Ky., and Novamed Surgery Center in New Albany, Ind., says his main concern about this approach is that Dr. Michelson’s considerable surgical and clinical skill and experience might give him an advantage some other surgeons couldn’t match, leading to less predictable results in their hands.
 “As a cornea, cataract and refractive specialist, I, too, look at mires from topographies and handheld keratoscopes every day in the OR and the clinic,” says Dr. Piracha. “I’ve found that the keratoscope is helpful with large amounts of astigmatism and irregular astigmatism, but when treating low degrees of regular astigmatism—i.e., less than 3 D—it’s very difficult to locate the axis of astigmatism accurately, as compared to topography or tomography. So I might use the keratoscope in real time when performing limbal relaxing incisions or astigmatic keratotomy in the former cases, but I’d rely on my automated measurements when implanting a toric lens in eyes with regular or low astigmatism. I’d only use the keratoscope to confirm that my axis was correctly marked. For the amount of astigmatism that toric IOLs can currently treat—up to 2 D—I think that a handheld keratoscope does not provide a level of detail and accuracy that would be of significant help.”
“As a cornea, cataract and refractive specialist, I, too, look at mires from topographies and handheld keratoscopes every day in the OR and the clinic,” says Dr. Piracha. “I’ve found that the keratoscope is helpful with large amounts of astigmatism and irregular astigmatism, but when treating low degrees of regular astigmatism—i.e., less than 3 D—it’s very difficult to locate the axis of astigmatism accurately, as compared to topography or tomography. So I might use the keratoscope in real time when performing limbal relaxing incisions or astigmatic keratotomy in the former cases, but I’d rely on my automated measurements when implanting a toric lens in eyes with regular or low astigmatism. I’d only use the keratoscope to confirm that my axis was correctly marked. For the amount of astigmatism that toric IOLs can currently treat—up to 2 D—I think that a handheld keratoscope does not provide a level of detail and accuracy that would be of significant help.”
Dr. Michelson admits the surgeon must have a keen eye. “You’ve got to be able to look at the rings projected by the video keratoscope and not only determine the axis of astigmatism, but also gain an idea of how elliptical the reflection is and how much astigmatism this represents,” he says. “It does take a little bit of a trained eye to see the axis in lower amounts of astigmatism, but it’s not that difficult, and it gets easier with practice. And of course, the more astigmatism the eye has, the easier the alignment becomes.”
Getting Started
“If a surgeon is interested in trying this approach, I recommend buying the device for a couple hundred dollars,” he says. “Just bring it into the OR and start looking at eyes. See if you can find the astigmatism, and keep practicing until you feel comfortable with it. If you want to mark the patient in advance using standard marking techniques, that’s fine. Use the keratometer when you start the surgery and see if it correlates with the marks you made. It only takes about 20 seconds to try it, and if you find that you can see the astigmatism on the keratometer, you may decide to wean yourself off of preoperative marking. I haven’t marked a patient for toric lenses in two or three years.”
Dr. Michelson notes that he’s not advocating change. “If you get good results doing it a different way, there’s no need to switch,” he says. “I’m comfortable with this technique because number one, I don’t have to worry about cyclotorsion, and number two, I don’t have to pre-mark, so it saves time. Basically, it’s an inexpensive way to line up the toric axis. It’s not magic, but it works.”