Today, cataract surgeons are seeing an increasing number of patients who underwent refractive surgery at some point in the past 35 years. It’s well known that the corneal alterations caused by refractive surgeries can make the calculation of intraocular lens power extremely challenging. But these patients also raise issues about what choice of intraocular lens will work best and what kind of refractive target will most effectively manage the problems associated with surgeries such as radial keratotomy. Here, four surgeons share what they’ve learned about getting the best results for patients who have had previous refractive surgery.
Spherical Aberration
Prior to wavefront technology, most refractive procedures induced positive spherical aberration. For that reason, aspheric IOLs are a good choice for many of these patients. “Correcting positive spherical aberration produces a 30- to 40-percent improvement in contrast sensitivity,” notes Jack T. Holladay, MD, MSEE, FACS, clinical professor of ophthalmology at Baylor College in Houston. “So, a key to managing these patients is measuring the cornea and determining the amount of spherical aberration—the Zernike (4,0) term—which is easily done with most topographers and tomographers. That way you can determine which aspheric lens is most appropriate to help offset the increased aberration.”
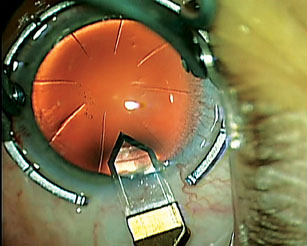 |
| A clear corneal cataract incision needs to avoid intersecting prior RK incisions. In some cases, a scleral-corneal tunnel may be necessary. (Photo courtesy Uday Devgan, MD, FACS) |
“The average spherical aberration in the normal human population is +0.27 µm of positive spherical aberration over a 6-mm pupil,” he continues. “That’s why the Tecnis lens was designed to have -0.27 µm of negative spherical correction. Individuals who had myopic LASIK or PRK before the advent of wavefront-guided and wavefront-optimized treatments ended up with some increase in spherical aberration; but if they had RK, their resulting spherical aberration could be as high as 0.4 or 0.5 µm. Unfortunately, no IOL is designed to correct that much spherical aberration—although the Tecnis can correct a lot of it.
“The exception to the increase in positive spherical aberration is the individuals who had hyperopic LASIK or PRK before the development of wavefront technology,” he adds. “By making their corneas steeper than before, these procedures actually induce negative spherical aberration. If enough was induced to reduce their spherical aberration to zero, then the Bausch + Lomb lens would be a good choice. If they turn out to have negative spherical aberration in the cornea, a standard spherical IOL would be a good choice; it will move you back a little bit in the positive direction.”
Uday Devgan, MD, FACS, chief of ophthalmology at Olive View UCLA Medical Center, associate clinical professor at the UCLA School of Medi-cine, and in private practice at Devgan Eye Surgery in Los Angeles, notes an important caveat to this strategy. “You have to make sure there are no other aberrations from the prior surgery,” he points out. “For example, if a prior LASIK ablation was slightly decentered or irregular—which you can typically see on topography—you might be better off with a zero spherical aberration lens, like the Bausch + Lomb SofPort AO or Akreos lens, or a Staar aspheric. These lenses induce almost no spherical aberration.”
Correcting Astigmatism After RK
Because RK both distorts and weakens the cornea, it raises several issues in regard to correcting any astigmatism you find. “Depending on the number of incisions and the size of the central clear zone, RK eyes often have components of both regular and irregular astigmatism,” notes Samuel Masket, MD, clinical professor of ophthalmology at the David Geffen School of Medicine, Jules Stein Eye Institute, at the Uni-versity of California, Los Angeles. “Furthermore, the cornea may be changed unpredictably as a result of cataract surgery. Unfortunately, when it comes to correcting astigmatism in a former RK patient, we only have two choices: either using surface laser ablation postop or toric IOLs intraoperatively. The post-RK eye doesn’t allow for astigmatic keratotomy, unless it’s a four-incision surgery. So typically, a limbal relaxing incision is off the table.”
“Because RK often induces astigmatism, you’d think a toric lens might be a good choice,” says Dr. Devgan. “But you have to be careful. In many cases a toric lens is not a great idea because the astigmatism induced by RK can be non-symmetric and irregular. You have to make sure that any astigmatism in the cornea is symmetrical, regular and stable before choosing a toric lens.”
Nevertheless, Dr. Masket believes that toric IOLs are sometimes the best option in these eyes. “I’ve had success with both laser ablation and toric IOLs, although you can have failures as well because of the unstable nature of the cornea,” he notes. “If there’s a fairly reproducible degree of astigmatism topographically on several occasions prior to surgery, and it’s a significant amount, and the patient is motivated and understands the possibility that the toric lens may not work, then I have no problem with implanting one. I believe the most important consideration is corneal stability.” He adds that there are pros and cons to using postop laser ablation to correct the astigmatism. “The downside,” he says, “is that it adds significantly to the expense and morbidity of the treatment. The good thing is that we can also deal with optical surprises or undesirable optical outcomes.”
James P. Gills, MD, founder and director of St. Luke’s Cataract & Laser Institute, and clinical professor of ophthalmology at the University of South Florida, says he would consider using a toric for a previous refractive surgery patient if the patient has a lot of astigmatism and it has a regular pattern. “People who have had a lot of RK—16 or 24 cuts—can have extremely variable astigmatism,” he notes. “Nevertheless, a toric lens might be a good choice if the astigmatism is very symmetrical. And a toric can sometimes work even if the symmetry isn’t perfect; we recently published a case in which a toric lens got great results even though the patient had a somewhat asymmetrical butterfly.”
Dr. Masket agrees that perfect symmetry isn’t always a prerequisite for using a toric lens. “Any patient who has paid for refractive surgery is a motivated individual in terms of spectacle independence,” he notes. “He’s likely to have a better understanding of the process and higher goals in terms of achieving it. That makes him a better candidate, even if the optical results are less predictable.”
RK: Working the Day Shift
Dr. Holladay notes that one challenge with targeting an IOL power for a post-RK patient is that these individuals often experience a shift in their refractive power during the day. “In the morning, because the cornea is swollen, vision will be more hyperopic,” he explains. “Over the course of the day, these patients may undergo a 1-D or 1.25-D myopic shift. So, if you target them to be emmetropic in the morning so they can drive into work without glasses, when they drive home they may be -1.25 D and need a pair of glasses. However, in my experience, this target is the best postop goal, because if you make these patients plano in the afternoon, then in the morning they can’t read or see distant objects without glasses.”
Dr. Masket notes that some of his patients have a specific task they perform at the same time most days, so he tries to accommodate that. “For example,” he says, “if they read on the computer most of the afternoon, I take their presurgical measurements in the afternoon so I can come as close as possible to matching their optical goal at that time of day.”
“These individuals adjust their schedules based on when they know their vision will be best,” observes Dr. Devgan. “So, you probably should aim for keeping them the same way. If they rely on a little bit of morning myopia for better reading, then you’d better make sure they’ll be a little myopic in the morning. If that’s not possible, at least let them know that you won’t be able to achieve that.”
Whatever your strategy for keeping the patient happy, Dr. Masket suggests measuring the cornea and refraction several times before surgery at different times of day to see the degree of corneal instability. “We typically measure in the morning and in the late afternoon,” he says. “That helps me determine what options are most likely to be successful.”
“The other important thing to remember,” adds Dr. Holladay, “is that you need to explain to the pa-tient preoperatively that cataract surgery won’t eliminate the fluctuation in vision caused by the RK, or for that matter, any haloes or glare that already existed before the cataract.”
The Gift That Keeps on Giving
Another problem associated with previous RK patient is that the patient’s refraction is likely to shift slowly over a period of years—both in terms of spherical refraction and astigmatism. “When you make a radial keratotomy, you’ve weakened the cornea,” says Dr. Holladay. “That weakness progresses over time—an effect you don’t see with LASIK or PRK. So the RK patient will have progressive hyperopic shift over the course of his life, and gradually increasing against-the-rule astigmatism.
“When you do the cataract operation, you want to try to address these issues,” he continues. “First, target a little on the myopic side to help offset the gradual hyperopic shift. Second, make sure you don’t induce against-the-rule astigmatism, because that’s already going to get worse over time. If against-the-rule astigmatism already exists, you can choose a toric IOL, perhaps aiming for a slight overcorrection, and/or do a limbal relaxing incision. However, you have to be careful.
“Let’s say the person originally had 3 D of with-the-rule astigmatism,” he says. “The RK surgeon got him down near plano with 1 D of with-the-rule astigmatism left. In that situation you wouldn’t want to do anything except put in a spherical IOL, because that residual with-the-rule astigmatism is going to continue to fade, go through zero and then become a little against-the-rule. If you correct that 1 D today, the patient will eventually end up with more against-the-rule astigmatism. Leaving a small amount of with-the-rule astigmatism will help him over the next five years.
“Where you place your cataract in-cision will be part of that equation, of course, because wherever you put the incision, the meridian will get flatter,” he adds. “A temporal incision, which is becoming more and more common, will reduce any existing against-the-rule astigmatism or increase any existing with-the-rule astigmatism, and you should take that into consideration.”
Dr. Devgan agrees that aiming for a little bit of residual myopia makes sense. “RK tends to push towards hyperopia for many years, or even decades,” he says. “In fact, many of these eyes ended up post-RK with a little hyperopia anyway, because most RKs were done to correct myopia, and postop errors in refractive surgery tend to fall opposite the original refractive error.”
Dr. Masket, however, says he doesn’t attempt to compensate for possible future shifts in RK patients’ astigmatism. “In my experience, this is unpredictable,” he explains. “I treat the astigmatism as the exam shows it, as long as it’s regular astigmatism and the amount and axis are stable over the course of two or three exams. The only thing that’s predictable in the post-RK patient is a progressive corneal flattening, and even in that case, the patient’s cornea may have stabilized by the time you see him, if he had the surgery 20 years earlier.”
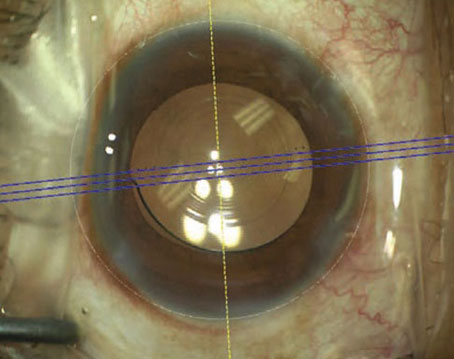
 |
| Cataract surgery after prior LASIK can lead to punctuate keratitis and dry eye. (Photo courtesy Uday Devgan, MD, FACS) |
Although aberration and fluctuation issues are far less of an issue with patients who’ve had PRK or LASIK, some issues can still arise—beyond the challenges of power calculation—when choosing a target refraction.
One of those issues is the need to plan ahead in terms of postop enhancement limitations. “When you’re doing an IOL on a post-LASIK eye, it’s important to remember that your lens calculations will be less accurate,” Dr. Devgan points out. “So you have to consider what your options will be if you need to enhance the result. If the patient had prior myopic LASIK, is there enough tissue to do a little more laser? If it was a +4 hyperopic LASIK, you’d better make sure the patient doesn’t end up more hyperopic, because you can’t do much more hyperopic LASIK. You could, however, do a little myopic correction.”
In theory, the previous LASIK or PRK will have eliminated most astigmatism, but that’s not always the case. “Normally, LASIK aims to get rid of corneal astigmatism because the corneal astigmatism tends to closely match the overall refractive astigmatism,” observes Dr. Devgan. “However, it’s possible that a patient could have had lenticular astigmatism prior to LASIK which was corrected by creating opposite astigmatism in the cornea to cancel it out. In that situation, taking out the lens during cataract surgery unmasks the laser-
induced corneal astigmatism. A pa-tient like that may require a toric lens.
“The other time to be careful with toric lenses is in patients with prior hyperopic LASIK,” he adds. “I’ve had cases in which the topography and keratometry misread the smaller-than-expected optical zone, so a toric IOL would have overcorrected the patient. For that reason, in cases with large hyperopic ablations and smaller optical zones, a non-toric IOL may be a better choice. Then, if the patient has significant astigmatism postop, that can be addressed then.”
 |
Some recent advances in lens optics are also showing promise in patients with corneal aberrations—whether from previous refractive surgery or other causes. In these patients, Dr. Gills favors using a biaspheric lens, in which both the front and back surfaces of the lens are aspheric; he says this dramatically reduces the impact of corneal aberrations. (Among these lenses, he favors Lenstec’s Softec HD, in which he has a financial interest.)
“Because both the front and back surfaces of the lens are aspheric, the light rays pass through the lens parallel to each other,” he explains. “The result is similar to the clarity you get with the pinhole effect; aberrations in the peripheral cornea have less effect on the fovea. For patients with previous RK, LASIK, hyperopic LASIK or hex-K—even basement membrane disease, nodules or keratoconus—these lenses work extremely well. For that reason, this is the only lens I like to use when a patient has had previous refractive surgery.” (Dr. Gills notes that one of the toughest groups to manage is patients who’ve had hyperopic LASIK. “These patients don’t get great results with any form of lens, but we’ve had the best results with biaspherics,” he says.)
Dr. Gills notes another benefit. “Because this lens cuts out the peripheral spherical aberrations, it eliminates glare,’ he says. “In fact, in a survey of patients at our clinic who received biaspheric lenses, 98.4 percent said their postop vision was as good as it had ever been, and half said it was better vision than they’d ever experienced.” Dr. Gills adds that he’s found this type of lens to be the best fit for previous RK patients. “I’ve replaced several other IOLs with biaspheric lenses, and these patients have had marked improvement in visual acuity and subjective vision,” he says.
However, Dr. Gills urges caution when managing astigmatism. “We find that existing astigmatism is mitigated by the biaspheric lens, so we don’t have to do as much correction as we would have expected based on preop measurements,” he says. “We’ve had previous refractive surgery patients with 2 or 3 D of astigmatism who had no measurable astigmatism after putting in a biaspheric lens. In most cases, it reduces the amount by half. For that reason, we wait until after implantation to treat the astigmatism.”
Management Strategies
Several other tactics can increase the likelihood of success with post-refractive surgery patients:
• Be wary of multifocal lenses. “RK patients, and those who had myopic LASIK or PRK more than five years ago, shouldn’t get a multifocal lens,” notes Dr. Holladay. “They’ve already had a contrast sensitivity loss from the refractive procedure, and a multifocal lens will make that worse. The exception would be patients who’ve had LASIK or PRK in the past five years, if there’s no irregular corneal astigmatism. Patients in that situation tend to be essentially the same as patients who haven’t had prior refractive surgery. Those people can get multifocal IOLs—assuming they are good candidates in the first place.”
Dr. Masket agrees. “I’ve occasionally implanted a multifocal in a previous RK patient with success, but only in patients with four incisions or less, a large optical zone and stable corneal curvature measured at different times during the day. The key to success is individualizing and involving the patient in the decision-making process.” (Dr. Masket notes that if a patient has become accustomed to monovision, either by hyperopic or myopic ablation, he prefers to try to match the monovision rather than switching to presbyopic lenses.)
• Use the contact lens method when determining refraction. “In a patient with previous refractive surgery, we use wavefront measurement, topography and the contact lens method to determine the refraction,” says Dr. Gills. “I usually aim to be closest to the contact lens refraction. Many doctors don’t use the contact lens method because it takes a lot of extra time, but in our practice, it’s absolutely mandatory in cases of previous refractive surgery.”
• Use accommodating lenses judiciously. “When implanting an accommodating lens such as the Crystalens, one of the largest concerns is the 5-mm optic,” notes Dr. Masket. “The small optic size means there’s great potential in the post-RK eye for additional edge glare at night. I think this type of lens is probably not a good idea, given the unpredictability of the optical outcome, the fluctuation of vision and the size of the optic.”
“If I choose to go with an accommodating lens, I’d put in the Crystalens AO, which has zero spherical aberration—not the HD,” adds Dr. Devgan. “The HD model has a little central zone which can cause the lens to create the same kind of difficulties as a multifocal might in these eyes.”
• Focus on patient counseling. Dr. Masket says the most important factor when dealing with a previous refractive surgery patient is counseling. “I always involve the patient in my thought process when we consider what type of lens I’ll implant, what the goals of surgery are, and our ability to reach those goals,” he explains. “The postop RK patient needs to be aware that the early postop results may not match the long-term optical result. The patient also needs to understand the uncertainties involved in determining which lens power will work best in his post-RK eye, and that we may have to enhance the result to achieve the best possible visual outcome. Previous LASIK and PRK patients also need to know that our ability to hit the optical target is reduced, and that they may require a touchup with surface laser ablation.”
• Warn patients about postop dry eye. “I warn these patients about the possibility of dry eye before proceeding,” says Dr. Devgan. “If they do develop dry eye, they’ll think you’re smart for predicting it. If you don’t forewarn them and it happens, you’re a bad guy for causing it.”
• Manage RK patients differently during surgery. Dr. Masket notes that previous RK patients do better when certain extra steps are taken. “During the surgery,” he says, “we lower the infusion height of the bottle and do our best to be as kind to the cornea as we can, minimizing mechanical trauma. Typically, I perform 2.2-mm micro coaxial phaco, which induces as little astigmatism as possible. I can use a clear corneal incision in patients who’ve had up to 12 RK incisions, but when you get to 16 or more RK incisions, you have to resort to a scleral-corneal tunnel.”
• Postpone enhancements for post-cataract RK patients until the eye is stable. “Postop, I take frequent corneal curvature measurements and perform topographical analysis and refraction to determine when the cornea is stable,” says Dr. Masket. “I wait for the point at which the K-reading and topography most closely resemble the preoperative corneal curvature, power and astigmatism. These can vary significantly from the early postop period to later on, because there’s a tendency for the cornea to flatten right after surgery as a result of the surgical trauma. The normalizing period may take weeks or months, varying with the number of RK incisions and the size of the clear zone. Once the cornea is stable, we can reassess the optical result and consider whether enhancements are necessary. Again, the patient needs to be fully aware of all of these pitfalls.” REVIEW
Dr. Devgan is a consultant for AMO and Bausch + Lomb, a speaker for Alcon, and former consultant for STAAR. Dr. Gills has a financial interest in Lenstec’s Softec HD intraocular lens, and in Allergan, Alcon and AMO. Dr. Masket is a consultant to Alcon Labs and receives speaking honoraria from Bausch + Lomb. Dr. Holladay is a consultant for AMO, NIDEK, Oculus, Acufocus, Allergan, Zeiss and Wavetec.